In today’s medical world, almost everyone talks about the most recent “scan” that they had at the hospital. These scanning devices make detailed pictures of internal body structures that cannot otherwise be seen without performing surgery. CaT scans (computed tomography) use X-rays, MRI scans (magnetic resonance imaging) use a magnetic field and radio waves, ultrasound tests use sonic waves, and bone scans use radioactive markers to image and mark areas of interest in the patient. These scans can show abnormalities in patients, however, current methods in histology are often required to confirm specific diagnoses. This is required in order to determine the patient treatment and prognosis.
In histology what are we looking for in the final slide?
Virtually every specimen that comes through the histology laboratory is routinely processed into a paraffin block, and a hematoxylin and eosin (H&E) slide is made. Pathologists are trained to render diagnoses by reviewing H&E slides. Even when frozen sections are made, at least one slide is stained with H&E.
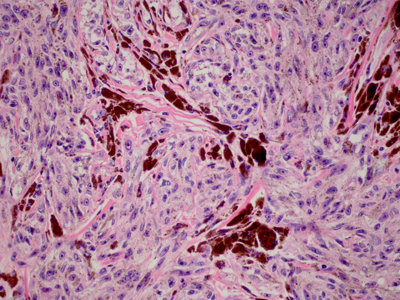
Hematoxylin stains nuclei and nuclear material varying shades of blue, while eosin stains red blood cells and connective tissue varying shades of pink. The resulting tinctorial patterns are evaluated by a pathologist to render a diagnosis.
In Figure 1, a skin section shows malignant melanoma cells in a spindle cell form, including dark brown melanin deposition. If this original specimen was received as an excisional procedure, the surgical margins would have been inked during the surgical grossing procedure. In this way, the pathologist can also assess the surgical margins and advise the clinician as to whether more tissue must be removed from the patient. Malignant melanoma is a skin cancer that must be completely removed in order to cure the patient. Any malignant melanoma cells left behind in the patient may metastasize to other organs, ultimately causing the patient’s death.
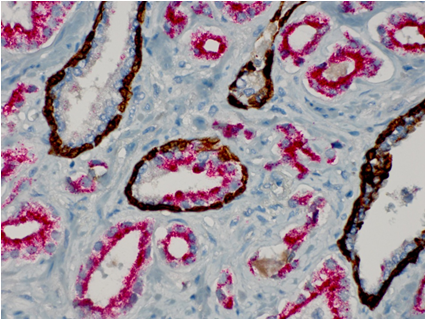
There are times when the H&E slide does not provide enough information to make a complete diagnosis. In these instances, additional procedures such as immunohistochemistry (IHC) need to be performed. While the H&E and other special stains rely on tinctorial results for evaluation, IHC uses specific antibodies to bind and localize specific proteins that may be present in the tissue section.
Figure 2 shows a section of prostate tissue from a prostate needle biopsy, in which the H&E slide did not show prostate cancer – but was suggestive of it. An IHC stain named “PIN 4” was performed, to show any “prostatic intraepithelial neoplasia (PIN) and/or any prostate carcinoma. This stain utilizes a “cocktail” of different antibodies to demonstrate basal layers in the prostate (dark brown) along with any neoplastic and/or cancer cells (red chromogen). The abundance of red staining in the figure clearly demonstrates the presence of proteins that are made by prostate cancer cells.
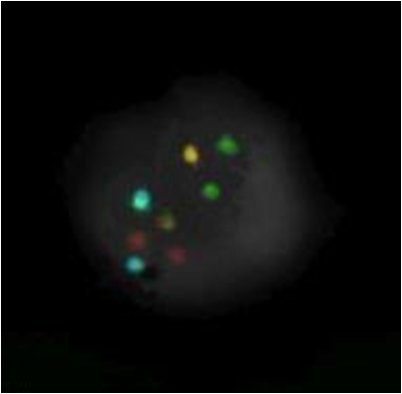
While IHC techniques use antibodies to localize specific proteins made by cells, the fluorescence in situ hybridization (FISH) procedure uses labelled probes to bind to specific sites within the nuclei of cells. Figure 3 shows one nucleus of a malignant melanoma cell binding four different colored probes. The probes are made to bind on specific DNA sequences on chromosomes. The probes are labelled with fluorescent tag molecules which fluoresce different colors when excited by different wavelengths of ultraviolet light. In this way, information can be obtained regarding the presence or absence of aberrant genes within the nucleus. This information can then be used to help establish specific diagnoses.
In summary, we can see that the histology laboratory has at its disposal an arsenal of routine and special procedures to probe the structure, function and genetic make up of cells obtained from the human body. This information is vital in helping determine patient diagnoses, treatment, and ultimate prognosis. In addition, the use of proper surgical grossing techniques on dermatopathology specimens (i.e. inking of surgical margins) help establish if all cancer cells have been removed, thereby helping to ensure patient survival.